Background
Dendritic cells are nonlymphoid, nonphagocytic, antigen-presenting cells present in lymphoid and nonlymphoid tissue. There are 4 types of dendritic cells: follicular, interdigitating, Langerhans, and fibroblastic cells. The WHO 2022 classification system groups dendritic cell and histiocytic neoplasms into 3 categories: plasmacytoid dendritic cell neoplasms, Langerhans cell and other dendritic cell neoplasms, and histiocytic neoplasms. The 2nd category is subdivided into “Langerhans cells neoplasms” and “other dendritic cell neoplasms”, which contains indeterminate dendritic cell tumor (IDCT) and interdigitating dendritic cell sarcoma (IDCS). The 2022 classification eliminated follicular dendritic cell sarcoma (FDCS) as it is no longer thought to be of hematopoietic origin. A prior Surveillance, Epidemiology, and End Results (SEER) review published in 2013 by Perkins and Shinohara grouped FDCS and IDCS and included 20 cases of IDCS diagnosed between 2001 and 2008. To our knowledge, this is the first update of epidemiologic and survival data for non-Langerhans cell and non-plasmacytoid dendritic cell neoplasms since the WHO reclassification.
Methods
We used the SEER 22 database, which collects data from cancer registries covering approximately 47.9% of the U.S. population. We selected all patients with cancers falling in the “other dendritic cell neoplasms” category according to the WHO 2022 classification from 2000-2020 using International Classification of Diseases for Oncology edition 3 (ICD-O-3) code of 9757/3, which codes for IDCS but also includes IDCT. The Kaplan-Meier method was used to display the survival curves. The Cox proportional hazards model was used to determine p values.
Results
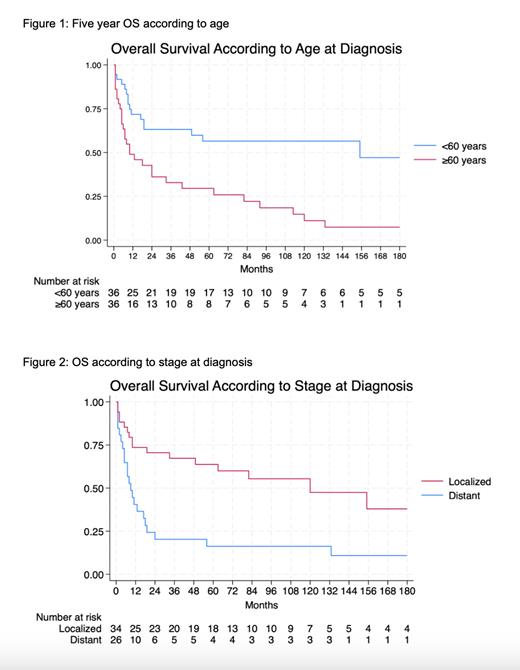
A total of 72 cases of IDCS/IDCT were identified. Median follow up was 19 months and median OS for the entire cohort was 24 months (95% CI 10-92 months). Of these patients, 61.1% (n=44) were White, 16.7% (n=12) were Hispanic, 13.8% (n=10) were Black, 5.6% (n=4) were Asian or Pacific Islander, and 2 patients were of unknown race. IDCS/IDCT was more common in males than females with a ratio of 1.77. The most common primary sites of involvement were connective tissue in 40.2% (n=29), head and neck in 16.7% (n=12), lymph nodes in 11.1% (n=8), and bone marrow in 8.3% (n=6). Patients with bone marrow involvement had a trend towards worse OS (median OS of 5 months). IDCS/IDCT is more common in adults but does occur in children and adolescents. Only 6 cases were diagnosed in patients under the age of 20 years. Patients who were under the age of 60 years at diagnosis had a median OS of 155 months compared to a median OS of only 10 months for patients who were 60 years or older at diagnosis (Figure 1, p<0.001). Staging was unknown in 12 patients. Of patients with known staging, 56.7% (n=34) had localized disease and 43.3% (n=26) had metastatic disease. Patients with localized disease at diagnosis had a better prognosis with a median OS of 120 months compared to 5 months for patients with metastatic disease at diagnosis (Figure 2, p<0.001). Treatment modality was unknown in 29 of the patients. Of patients with known treatment, 34.9% (n=15) had surgery alone, 20.9% (n=9) had chemo alone, 16.3% (n=7) had radiation alone, and 27.9% (n=12) had combination treatment. Single modality treatment regimens were most popular in patients with localized disease with 48% (n=12) of the patients with known treatment modality getting surgery alone, followed by radiation alone at 24% (n=6).The most common cause of death in this cohort was IDCS/IDCT with 76% of deaths being attributed to the cancer (n=35, there were 46 total deaths).
Conclusions
Though cases of IDCS and IDCT have more than tripled since 2008, it still remains the rarest type of dendritic cell neoplasm. Connective tissue, head and neck, and lymph nodes were the most common sites involved. Surgical resection was the most common treatment modality followed by chemotherapy. Clinical presentation is rare in patients under the age of 20 years. Age 60 years and older and metastatic disease were associated with poor outcomes with a signal towards worse survival when bone marrow was involved. Our study updates current knowledge of IDCS/IDCT and highlights some of the unknowns in this type of neoplasm, particularly regarding other prognostic factors including treatment effect on survival.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal